About one half of all pregnancies in the United States are unplanned. Most women can become pregnant from the time they are in their early teens until they are in their late 40s. Birth control can help couples postpone having a baby until the time is right for them—if ever. Some types of birth control also help protect against sexually transmitted diseases (STDs). Today, there are many choices of birth control for women and men.
How Birth Control Works
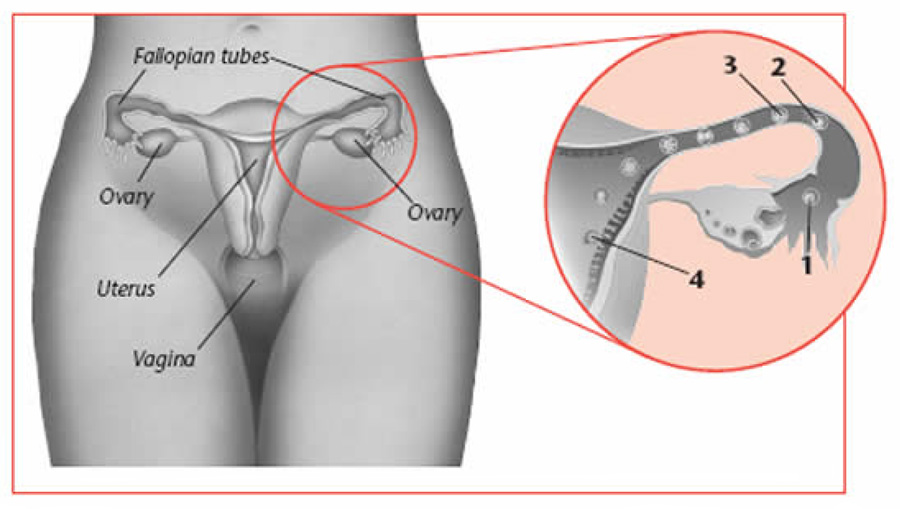
To understand how birth control works, it is important to know what happens during reproduction. A woman has two ovaries, one on each side of the uterus. Each month, one of the ovaries releases an egg into a fallopian tube. This is called ovulation. In most women, it occurs about 12–14 days before the start of the menstrual period.
A woman can get pregnant if she has sex around the time of ovulation. During sex, the man ejaculates sperm into the vagina. The sperm travel up through the mucus of the cervix, through the uterus, and into the fallopian tubes.
If a sperm joins with an egg in a fallopian tube, fertilization occurs (see figure on page 2). The fertilized egg then moves down the fallopian tube to the uterus where it can attach and grow in the endometrium (lining of the uterus).
Birth control methods work in a number of ways. They may:
- Block the sperm from reaching the egg
- Kill or damage sperm
- Keep eggs from being released each month
- Change the lining of the uterus so the fertilized egg does not attach to it
- Thicken the mucus in the cervix so sperm can not easily pass through it
Protect Yourself
You can reduce the risk of STDs, including HIV, if you:
- Know your partner. It is not just your own behavior that puts you at risk for infection—it is your partner’s too. Ask about his sexual history and whether he has ever used intravenous (IV) drugs.
- Limit sex partners. The more partners you or your partners have, the higher the risk of getting an STD.
- Use a latex condom. Proper condom use helps protect you and your partner from infection with STDs.
- Avoid risky sex practices. Sexual acts that tear or break the skin or
mucus membranes carry a higher risk of STDs.
Even small cuts that do not bleed let germs in and out. Anal sex poses a high risk because tissues in the area of the rectum break easily. Oral sex also may pose a risk.
Choosing a Method
There are many types of birth control, including barrier methods, hormonal methods, IUDs, fertility awareness, and sterilization. Couples may find some methods of birth control meet their needs better than others. Here are some things to think about when choosing a method:
- How well the method works and the side effects
- How likely you are to use it according to the directions
- Your age and overall health
- How often you have sex
- Whether a prescription is needed
- Whether you want to have children later
- Whether it helps protect against STDs
Certain types of birth control also offer added health benefits. Discuss the pros and cons of each method with your doctor so you can choose the best method for you.
Effectiveness
Most women think that the most important thing about a birth control method is how well it protects against pregnancy. All methods have a chance of failure. When a method is used correctly each time, the failure rates are lower.
The “failure rate” for each method is the number of women who would get pregnant if 100 women used the method for a year. For example, the IUD has a failure rate of about 1%. This means that about 1 woman out of 100 would get pregnant in a year of using it. Condoms have a higher failure rate of about 15%, meaning 15 women out of 100 would get pregnant using them for a year. Without using any method at all for a year, about 85 women out of 100 would get pregnant.
Special Needs
Choosing a form of birth control is more complicated for women with special needs. Sometimes this has to do with a woman’s reproductive stage—whether she is a teen, breastfeeding, or in perimenopause, for instance. Some women have chronic health problems that need to be considered. Women with disabilities also face challenges. Talk to your doctor about which method may be best for you.
More than one type of birth control may be used at the same time, for instance birth control pills and condoms. This is one of the best ways to prevent pregnancy and STDs. If a condom breaks or if birth control was not used, emergency contraception is an option.
Emergency Contraception
If a woman has sex without any type of birth control or if she thinks her method did not work (for instance, a condom slipped or broke), she may want to use emergency contraception. Emergency contraception reduces the risk that pregnancy will occur. There are two types of emergency contraception available in the United States: Plan B and the IUD.
Plan B is a prescription of two pills, like birth control pills, that are taken 12 hours apart. You need to take them within 120 hours (5 days) of unprotected sex. They are 75–89% effective at preventing pregnancy. Plan B usually works by preventing ovulation. Plan B will not work if you are already pregnant and will not affect a pregnancy that has started.
If you are aged 18 years or older, Plan B can be bought in pharmacies without a prescription. If you are younger than 18 years and need Plan B, you need a prescription. Call your doctor’s office or go to a family planning clinic or hospital emergency room. If you need to find a doctor to get a prescription, call the Emergency Contraceptive Hotline (888-NOT-2-LATE).
Some doctors will give you an advance prescription for Plan B. This way, you will have it on hand if you need it. The sooner the treatment begins, the more effective.
If you use birth control pills as your regular method of birth control, you can take a certain number of pills for emergency contraception. The amount is different for each type of pill. Ask your doctor or pharmacist what the right number is for the type of pill you are taking.
Another option is to have a copper IUD inserted. The IUD must be inserted within 5 days of having unprotected sex. It is about 99% effective. A benefit is that the IUD can then be used for long-term contraception.
Barrier Methods
Barrier methods prevent the man’s sperm from reaching the woman’s egg. Types of barrier methods include condoms (male and female), spermicides, the sponge, the diaphragm, and, although less commonly used, the cervical cap and Lea’s Shield. Using a spermicide with a barrier method can help reduce the risk of pregnancy even more.
Condoms
Condoms come in male and female versions. The male condom is a thin sheath made of latex (rubber), polyurethane (plastic), or animal membrane that is worn by the man over his erect penis. Latex condoms also protect against STDs, including HIV.
The female condom is a thin plastic pouch that lines the vagina. It is held in place by a closed inner ring at the cervix and an outer ring at the opening of the vagina. The female condom can be difficult to insert, so it is best suited for women who cannot be sure their partner will use a male condom every time they have sex. The female condom can be inserted up to 8 hours before sex and reduces the risk of STDs.
When sperm is released, it stays inside the condom and does not pass into the woman’s vagina. Both types of condoms are more effective when used with a spermicide.
To be effective, condoms must be used every time you have sex and must be put on correctly (see box). A condom should be used only once and only one should be used at a time. A female condom should not be used with a male condom because both are more likely to break.
Spermicides
Spermicides often are used in suppositories, foam, cream, jelly, and film (thin sheets that contain spermicide) to kill sperm or make them inactive. Before each act of sex, spermicide is placed in the vagina close to the cervix. Some types of spermicide need to be placed in the vagina before sex so they have time to melt and become active. Be sure to follow the instructions supplied with the product. Frequent use of some spermicides may irritate vaginal tissue and increase the risk of STDs.
Spermicide can be used with all barrier methods except the sponge, which already contains a spermicide.
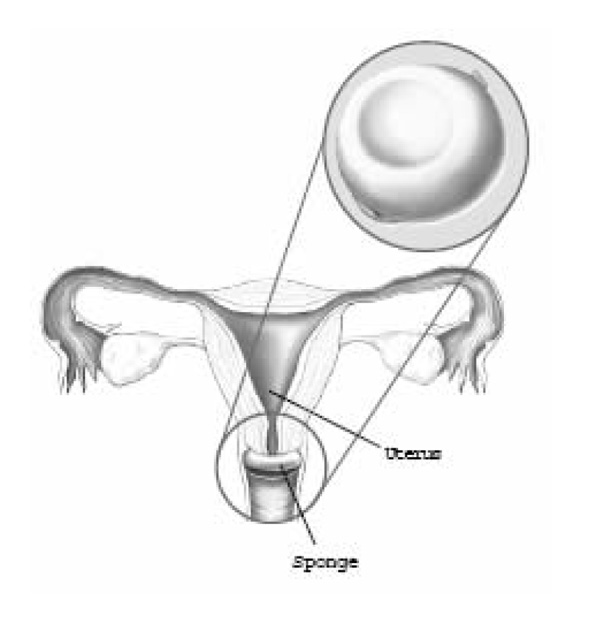
Sponge
The sponge is a doughnut-shaped device made of soft foam coated with spermicide. To use the sponge, it must be moistened with water. Once inserted in the vagina, it covers the cervix and blocks sperm from entering the uterus.
The sponge may be put in up to 24 hours before sex and should be left in place for at least 6 hours, but not more than 24 hours, after sex. During this time, it is good for more than one act of sex. The sponge should not be used during menstruation.
Diaphragm
The diaphragm is a small, latex, dome-shaped device that fits inside the vagina and covers the cervix. It is used with spermicide. A diaphragm requires a prescription and needs to be fitted by a doctor.
The diaphragm can be inserted up to 6 hours before sex. After sex, the diaphragm must be left in place for about 6 hours, but not more than 24 hours. Once inserted, the diaphragm stays in place and, if it is properly placed, cannot be felt.
A diaphragm is not reliable without spermicide. More spermicide should be used before each act of sex, no matter how closely timed they are. This can be inserted while the diaphragm is still in place.
Women using a diaphragm should practice how insert and remove it. Before the diaphragm is inserted, spermicidal cream or jelly should be applied around the rim and inside the dome of the diaphragm. It is then folded and inserted into the vagina. When the diaphragm is pushed up as far as it will go, the front part of the rim should be up behind the pubic bone. After the diaphragm is in place, the cervix should be completely covered by the rubber dome. You can feel to check if it is placed correctly. To remove the diaphragm, pull gently on the front rim.
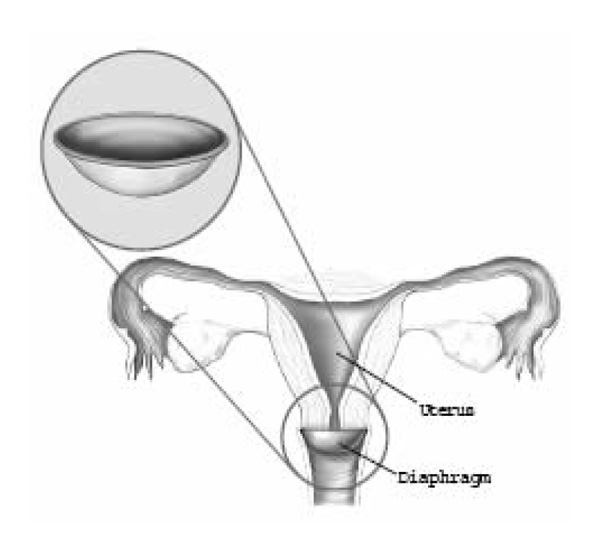
Women using a diaphragm also should learn how to care for it. To wash the diaphragm, use mild soap and water. Rinse the soap off well (it can damage the rubber), dry it, and put it back in its case. It should be checked monthly for holes. A diaphragm should be replaced about every 2 years.
Using the diaphragm may reduce the risk of some STDs. When the diaphragm is used with the male condom, it provides added protection from pregnancy and STDs. The diaphragm should not be used during menstruation.
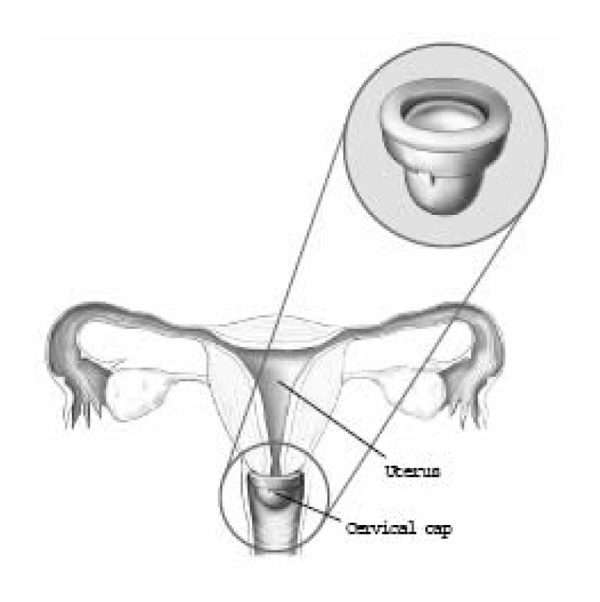
Cervical Cap
The cervical cap is a small, thin, dome-shaped device made of latex or plastic. If fits tightly over the cervix and stays in place by suction. A cervical cap must be fitted and prescribed by a doctor.
Like the diaphragm, the cap works better with a spermicide. Inserting a cervical cap is like inserting a diaphragm. Spermicide is place inside the cap, which is then squeezes and inserted into the vagina. The cap is then pressed onto the cervix until the cervix is completely covered. Before each act of sex, the cervix should be checked to make sure it is covered. This is done by pressing on the dome of the cap. Spermicide does not need to be reapplied before each act of sex. After sex, the cap should be left in place for 6 hours but not longer than 48 hours.
The cervical cap should not be used during menstruation.
Lea’s Shield
The Lea’s Shield is a dome-shaped silicone device with a loop for removal that fits inside the woman’s vagina and covers her cervix. It is used with spermicide.
The Lea’s Shield comes in only one size and requires a prescription. It has a one-way valve that creates suction that helps it fit against the cervix. The valve lets secretions flow out without letting sperm in.
The Lea’s Shield can be inserted anytime before sex. It must be left in place for at least 8 hours after sex, but should not be in place for more than 48 hours total. It can be reused and should be washed with soap and water between uses and be replaced as soon as it shows any signs or wear or weakness. The Lea’s Shield does not protect against STDs.
Hormonal Methods
With hormonal birth control, a woman takes hormones similar to those her body makes naturally. In most cases, these hormones prevent ovulation and change the lining of the uterus. The hormones also cause the cervical mucus to thicken, which makes it hard for the sperm to get through the cervix to the uterus. Hormonal birth control comes in several forms:
- Birth control pills
- Skin patch
- Vaginal ring
- Injections
- Implant
Hormonal Methods of birth control do not protect against STDs.
For most women, the risk of serious complications is small. However, women with certain medical conditions should discuss them carefully with their doctors. Methods that contain both estrogen and progesterone are not recommended for women older than 35 years who smoke cigarettes. A prescription is required for this type of birth control.
Birth Control Pills
There are many different brands of pills that use certain hormones or a combination of hormones. This variety allows a women to find a pill that is right for her.
Combination pills contain the hormones estrogen and progestin. Combination birth control pills offer health benefits to some women. They help protect against ovarian and endometrial cancer. Women who take birth control pills have shorter, lighter periods of bleeding (similar to that of a menstrual period).
Most pills come in packs of 28 pills. With this type of pill, one pill is taken at the same time each day for 28 days. When all the pills in the pack are finished, a new pack is started the next day. Bleeding occurs during the week when the last 4 or 7 pills are taken, depending on the type of pill.
Missing a period is common. If this occurs, the pills should be continued. Using birth control pills during pregnancy does not increase the risk of birth defects.
Side effects of the pill include nausea, breast tenderness, and headaches. They often go away after a few months of use. There will likely be fewer side effects if the pill is taken at the same time every day.
Progestin-only pills, sometimes called minipills, do not contain estrogen. This type of pill is a better choice for women who have certain health problems and cannot take pills with estrogen. It often is recommended for women who are breastfeeding. The progestin-only pill comes in packs of 28 pills. All the pills in the pack contain hormones. It is important not to miss a pill and to take it at the same time each day.
If you miss some pills, you may have some spotting or light bleeding even if you make up the missed pills. These side effects are not harmful.
Continuous-Dosing Pills
Continuous dosing (also called extended use) is a new option available in combination pills. With this method, instead of taking hormones for 21 days with 7 days off, you take hormones for 84 days with 7 days off. This means that you will have only four periods of bleeding in a year. There are also pills that comes in packs of 28, in which all the pills are active. This means that you will not have any bleeding.
Some women decide to take this type of pill simply because they want to have fewer or no periods. For others, this method can help with health problems that are affected by having periods, such as dysmenorrhea (painful periods), endometriosis, or fibroids. If you have fewer periods, you have fewer symptoms. Eventually most women who take these types of pills will not get periods.
It may take some time for your body to adjust to the constant levels of hormones. A common side effect, breakthrough bleeding (bleeding at a time other than your period), can happen on and off when you first start taking these pills. Over time, the number of these days often decreases.
If You Miss A Pill
You may forget to take a pill once in a while. To find out what to do, read the information that came with your pill pack or call your doctor or nurse. You may need to use a backup method of birth control (such as condoms) or emergency contraception.
Skin Patch
The contraceptive skin patch is a small (1.75 inch) adhesive patch that is worn on the skin to prevent pregnancy. With the patch, estrogen and progestin are absorbed through the skin into the bloodstream. The patch may offer many of the same benefits and risks as the combination birth control pill. Once a woman obtains a prescription for the patch, she does not need to visit her doctor to apply or remove it.
The patch can be worn on the buttocks, chest (excluding the breasts), upper back or arm, or abdomen. It should be applied to a new place each week to avoid irritation.
A patch is worn for a week at a time for a total of 3 weeks in a row. During the fourth week, a patch is not worn, and bleeding occurs. After week 4, a new patch is applied and the cycle is repeated. Although the patch starts working right away, a backup method of birth control, such as condoms, should be used for the first week of the first cycle. The patch may be less effective in women who weigh more than 198 pounds.
Vaginal Ring
The vaginal ring is a flexible, plastic ring that is placed in the upper vagina. It releases both estrogen and progestin. The ring may have the same benefits and risks as those of the combination birth control pill.
The ring is worn for 21 days, removed for 7 days, and then a new ring is inserted. During the week it is out, bleeding similar to that of a menstrual period occurs. A woman does not need to visit her doctor for insertion or removal of the ring, although a doctor must prescribe it.
To use the ring, it is folded and inserted into the vagina. This is all that needs to be done to place the ring in the correct position. After 3 weeks, the ring is removed on the same day of the week and around the same time that it was inserted.
Bleeding usually will start 2-3 days after the ring is removed. A new ring is inserted 1 week after the last one was removed.
Although this rarely happens, the vaginal ring can slip out of the vagina. If it has been out for more than 3 hours, a backup method of birth control should be used for 7 days. If the vaginal ring slips out often, a different method of birth control may be needed.
Pregnancy is prevented as it is with other hormonal methods. When a woman begins using the vaginal rind, she should use a backup method of birth control, such as condoms or spermicide, for the first 7 days of use.
Injections
An injection of “shot” of depot medroxyprogesterone acetate (DMPA) provides protection against pregnancy for 3 months. It works the same way as other forms of hormonal birth control.
A doctor or nurse gives the injection. After the first injection, a backup method should be used for the next 7 days. Injections may be good for people who find it hard to use daily birth control methods. Injections also may be good for women who cannot use combination birth control pulls or IUDs.
Some women using this method have irregular bleeding. Over time, many women stop bleeding altogether. Weight gain also may occur in some women. Many women and teenagers also have a decrease in bone density while using hormonal injections. Bone density appears to return to levels that are normal for the woman’s age group when the injections are stopped.
DMPA injections can be used when a woman is breastfeeding. A woman can start DMPA injections after giving birth. After a woman stops DMPA injections, fertility returns in about 10 months. But for some, it may take much longer. If a woman knows she wants to become pregnant within the next couple of years, she should choose another form of birth control.
Implant
A contraceptive implant is a single rod that is inserted under the skin of the upper arm. It protects against pregnancy for 3 years. The implant releases a progestin that works similar to other hormonal methods of birth control – it prevents ovulation.
The implant can be inserted and removed in a doctor’s office in about 5-10 minutes. The area where the implant will be placed is numbed with a local anesthetic. no incision needs to be made. A woman can become pregnant soon after the implant is removed.
The most common side effect of using a contraceptive implant is irregular bleeding. This side effect usually goes away in 6-9 months. Some women stop bleeding altogether.
Intrauterine Device
The IUD is a small, T-shaped, plastic device that is inserted and left inside the uterus to prevent pregnancy. There are two types available in the United States: the hormonal IUD and the copper IUD. The IUD does not protect against STDs.
The hormonal IUD releases a small amount of the hormone progestin into the uterus. This thickens the cervical mucus, which blocks sperm from entering the cervix. It also thins the endometrium. The hormonal IUD also may make the sperm less active and make the sperm and egg less likely to be able to live in the fallopian tube. This keeps a fertilized egg from attaching there or in the uterus.
The copper IUD releases a small amount of copper into the uterus. In most cases, this prevents the egg from being fertilized or, in rare instances, from attaching to the wall of the uterus. The copper also prevents sperm from going through the uterus and into the fallopian tubes and reduces the sperm’s ability to fertilize an egg.
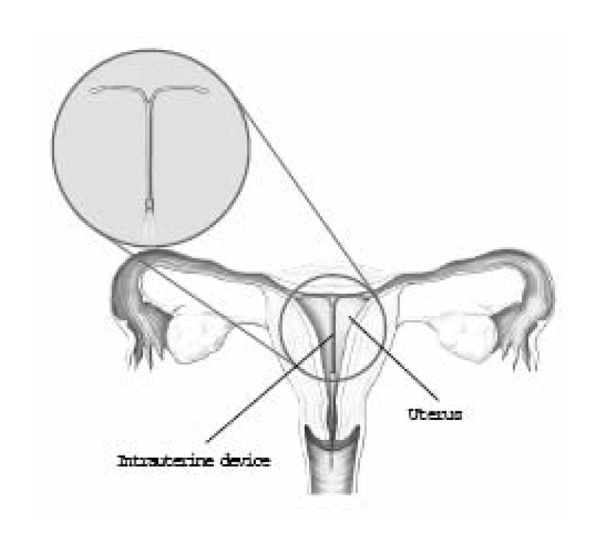
The hormonal IUD must be replaced every 5 years. The copper IUD can remain in your body for as long as 10 years. As soon as the IUD is removed, there is no protection against pregnancy.
A doctor must insert and remove the IUD. The insertion procedure may cause discomfort, but once it is in place, you do not have to do anything else to prevent pregnancy. It does not interfere with sex, daily activities, or menstruation. You can use a tampon with it. Physical activity will not move the IUD. You may be asked to return for a routine checkup after the IUD is inserted.
Each IUD comes with a string or “tail” made of a thin plastic thread. Placing a finger in the vagina to locate this string can check the placement of the IUD. If you cannot feel the string, call your doctor.
Menstrual pain and bleeding often increase with the copper IUD. Women who use the hormonal IUD often have less menstrual pain and bleeding. Some women using hormonal IUDs stop having periods altogether.
Some women have cramping and spotting during the first few weeks after the IUD is inserted. Vaginal discharge also can occur. These symptoms are common and should disappear within a month.
Serious complications from use of an IUD are rare. However, some women do have problems, usually during or soon after insertion:
- Expulsion. The IUD is pushed out of the uterus into the vagina.
- Perforation. Although rare, the IUD can pierce the wall of the uterus during insertion.
- Infections. Infections in the uterus or fallopian tubes can occur after insertion. This may cause scarring in the reproductive organs, making it harder to become pregnant later.
- Pregnancy. Rarely, pregnancy may occur while a woman is using an IUD. If the IUD remains in place, there can be risks to the mother and fetus, including miscarriage, infection, or preterm birth.
Fertility Awareness
Fertility awareness (sometimes called natural family planning) does not require drugs or devices. There are many methods of fertility awareness and the success or failure of any of these methods will depend on the woman’s ability to:
- Recognize the signs of ovulation
- Not have sex during the fertile period, or use another method, such as condoms, during that time
It is helpful to have training in the use of these methods. Natural family planning does not protect against STDs.
Ovulation/Cervical Mucus Method
The ovulation method involves changes in how much mucus is produced by the cervix and in how it feels. Women who use this method learn to recognize the changes that occur around the time of ovulation. To do this, a woman checks regularly for mucus at the opening of the vagina and assesses it for such changes.
Just before ovulation, the mucus of the cervix becomes thin and watery. The last day of thin and watery discharge occurs at the time of ovulation. Just after ovulation, the mucus becomes thick again. The ideal days for having sex when trying to prevent pregnancy are the 10 or 11 days at the end of the cycle and the discharge-free days (if any) that occur just after menstruation.
Symptothermal Method
The symptothermal method takes into account a woman’s body temperature and signs of ovulation. In addition to taking her temperature and checking for mucus changes, the woman checks for other signs of ovulation, such as abdominal pain or cramps, spotting, and any change in the position and firmness of the cervix.
This method requires that you do not have sex from the day you first notice signs of fertility (mucus or wet feeling) until the third day after the increase in temperature or the fourth day after the peak day of mucus production.
Lactational Amenorrhea
Lactational amenorrhea means a woman does not have her period because of a change in hormones caused by breastfeeding. Ovulation and menstruation usually do not occur in women who are breastfeeding who do not use formula to supplement feedings. If a woman does not ovulate, she cannot become pregnant.
This method is most effective during the first 6 months of exclusive breastfeeding. It loses effectiveness over time. A backup method may need to be used with it. Ovulation can occur without a menstrual period. However, once menstruation occurs, the risk of pregnancy is greatly increased.
Sterilization
Sterilization is a permanent method of birth control. The procedure for women is called tubal sterilization. The procedure for men is called vasectomy.
Sterilization is a major decision that should be made with care. Women and men who have this procedure should be certain that they do not want to have any more children—now or in the future. Reversing the procedure requires major surgery and is not always effective. If you plan to have a sterilization procedure, you may want to think about vasectomy for your male partner. It is a simpler procedure and has fewer risks.
Sterilization for Women
Tubal sterilization works by surgically blocking or cutting the fallopian tubes. Sterilization does not affect a woman’s menstrual cycle or sexual activity.
Tubal sterilization can be done in different ways. The two methods used most often are laparoscopy and minilaparotomy. Through a small cut, the fallopian tubes are closed by tying, banding, clipping, blocking, or cutting them, or by sealing them with electric current. Anesthesia is used with all methods, and a hospital stay is not required.
One form of sterilization does not involve surgery. For this procedure, a hysteroscope is placed through the cervix into the uterus and a tiny springlike device is inserted through the scope into each fallopian tube. The device causes scar tissue to build up, which blocks the fallopian tubes and prevents the sperm from reaching the egg. It takes 3 months for the scar tissue to grow, so women should use another method of birth control during this period. The woman then may need to have an X-ray test to be sure the fallopian tubes are blocked. The procedure can be done in a doctor’s office without anesthesia.
Some women have tubal sterilization right after giving birth. This is called postpartum sterilization. If you are having a cesarean birth, sterilization may be performed at the same time, without the need for an additional operation or a prolonged hospital stay.
You will need to consent to have a sterilization procedure. Depending on the type of insurance you have, you may have to wait for a certain number of days after signing a consent form before having the procedure done.
Sterilization for Men
A vasectomy works by blocking the tubes that carry sperm from the man’s testes to the penis (the vas deferens). This prevents the release of sperm. After a vasectomy, a man’s sexual function does not change. He can have an erection and ejaculate.
A vasectomy can be done in different ways. The vasa are tied, cut, clipped, or sealed through one or two small cuts in the skin of the scrotum. Some doctors use a “noscalpel” technique. This procedure cuts the vas deferens the same way, but instead of making an incision, a special tool is used to puncture the scrotum in one place. No stitches are needed after procedure. Both of these procedures may be done in a doctor’s office, clinic, or hospital.
A vasectomy is not effective right away. Some sperm may still be in the tubes. It often takes 2–3 months for the vasectomy to work. For this reason, a couple must still use a method of birth control until a return visit to the doctor or clinic for a final sperm count (in which the number of sperm in a semen sample are counted).
Finally
No matter which method of birth control you choose, be sure that you know how it works, how to use it, and what side effects may occur. Although some methods may not require a prescription or a visit to your doctor, you still need to learn how to use the method properly. A doctor, nurse, or family planning counselor can teach you. The more you know about birth control and your own needs, the easier it will be to choose a method that is right for you.
Resources
The Guttmacher
Institute 1301 Connecticut Avenue, NW Suite 700, Washington, DC 20036
Phone: (877) 823-0262
Fax: (202) 223-5756
Web Address: http://www.guttmacher.org
The American College of Obstetricians and Gynecologists
409 12th Street, SW PO Box 96920, Washington, DC 20090-6920
Phone: (202) 638-5577
Fax: (202) 484-5107
Web Address: http://www.acog.org/goto/patients
American Medical Association
515 North State Street, Chicago, IL 60610
Phone: (800) 621-8335
Web Address: http://www.ama-assn.org
Association for Reproductive Health Professionals
2401 Pennsylvania Avenue, NW Suite 350, Washington, DC 20037-1718
Fax: (202) 466-3825
Web Address: http://www.arhp.org
Centers for Disease Control and Prevention
1600 Clifton Road, Atlanta, GA 30333
Phone: (800) 311-3435
Web Address: http://www.cdc.gov
Institute for Reproductive Health Georgetown University
4301 Connecticut Avenue, NW Suite 310, Washington, DC 20008
Phone: (202) 687-1392
Fax: (202) 537-7450
Web Address: http://www.irh.org
MedlinePlus U.S. National Library of Medicine
8600 Rockville Pike, Bethesda, MD 20894
Phone: (888) 346-3656
Web Address: http://www.medlineplus.gov
National Women’s Health Network
514 10th Street, NW Suite 400, Washington, DC 20004
Phone: (202) 628-7814
Fax: (202) 347-1168
Web Address: http://www.nwhn.org
National Women’s Health Information Center
U.S. Department of Health and Human Services
Office on Women’s Health
Phone: (800) 994-9662
Web Address: http://www.4woman.gov
National Women’s Health Resource Center
157 Broad Street Suite 315, Red Bank, NJ 07701
Phone: (877) 986-9472
Web Address: http://www.healthywomen.org
North American Menopause Society
PO Box 94527, Cleveland, OH 44101
Phone: (440) 442-7550
Fax: (440) 442-2660
Web Address: http://www.menopause.org
Planned Parenthood Federation of America
434 West 33rd Street, New York, NY 10001
Phone: (800) 230-7526
Fax: (212) 245-1845
Web Address: http://www.plannedparenthood.org
Glossary
Anesthesia: Relief of pain by
Cervix: The lower, narrow end of the uterus, which protrudes into the vagina.
Cesarean Birth: Delivery of a baby through an incision made in the mother’s abdomen and uterus.
Endometriosis: A condition in which tissue similar to that normally lining the uterus is found outside of the uterus, usually on the ovaries, fallopian tubes, and other pelvic structures.
Erection: A lengthening and hardening of the penis.
Estrogen: A female hormone produced in the ovaries.
Fallopian Tube: One of two tubes through which an egg travels from the ovary to the uterus.
Fibroids: Benign growths that form in the muscle of the uterus.
Laparoscopy: A surgical procedure in which a slender, light-transmitting instrument, the laparoscope, is used to view the pelvic organs or perform surgery.
Minilaparotomy: A small abdominal incision used for a sterilization procedure in which the fallopian tubes are closed off.
Miscarriage: Early pregnancy loss.
Ovaries: Two glands, located on either side of the uterus, that contain the eggs released at ovulation and that produce hormones.
Ovulation: The release of an egg from one of the ovaries.
Penis: An external male sex organ.
Perimenopause: The period around menopause, which usually extends from ages 45 to 55 years.
Progestin: A synthetic form of progesterone that is similar to the hormone produced naturally by the body.
Scrotum: The external genital sac in the male that contains the testes.
Sexually Transmitted Diseases (STDs): Diseases that are spread by sexual contact.
Sperm: A male cell that is produced in the testes and can fertilize a female egg.
Testes: Two male organs that produce the sperm and male sex hormone.
Uterus: A muscular organ located in the female pelvis that contains and nourishes the developing fetus during pregnancy.
Vagina: A tube-like structure surrounded by muscles leading from the uterus to the outside of the body.
Vas Deferens: Two small tubes that carry sperm from the male testes to the prostate gland.
